Macular Degeneration
What is age-related macular degeneration (AMD)?
Age-related macular degeneration (AMD) is a common cause of visual loss in elderly people. It is divided into two categories: “dry” and “wet”. The macula is the central part of the retina, which is similar to the film in the back of a camera. If the central part of the film were damaged, the camera would not take good photographs. Similarly, in macular degeneration, the vision can become blurred. The figure to the right illustrates the sort of blurring that patients with macular degeneration often experience:
The following video describes how the eye works and how AMD can affect the vision:
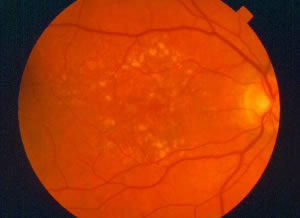 “Dry” AMD is the deterioration of the tissues beneath the retina, without any abnormal blood vessel growth. It is much more common than wet AMD; about 90% of AMD cases are dry. To better understand how dry AMD causes visual loss, think of the retina as a patch of grass. The retina is nourished by tissues beneath it, much like grass is nourished by soil. If the soil contains a lot of clay, the grass is not likely to grow well. Similarly, if the tissues beneath the retina deteriorate, they do not properly nourish the retina and the vision worsens. Most people with dry AMD maintain excellent vision. Only in the most advanced cases of dry AMD do people experience significant visual loss. Even people with advanced dry AMD can typically see well enough to function quite well. Tasks that require good detailed vision like reading, driving and recognizing faces, however, are difficult. Unfortunately, there is no widely accepted treatment for dry AMD. Vitamins are typically recommended in an effort to stabilize the vision, however. See “Vitamins and Other Nutritional Supplements” below for a discussion of vitamins. The photograph to the left shows typical dry AMD. Notice the numerous yellow dots; these are deposits beneath the retina known as drusen and are a hallmark of dry AMD:
“Dry” AMD is the deterioration of the tissues beneath the retina, without any abnormal blood vessel growth. It is much more common than wet AMD; about 90% of AMD cases are dry. To better understand how dry AMD causes visual loss, think of the retina as a patch of grass. The retina is nourished by tissues beneath it, much like grass is nourished by soil. If the soil contains a lot of clay, the grass is not likely to grow well. Similarly, if the tissues beneath the retina deteriorate, they do not properly nourish the retina and the vision worsens. Most people with dry AMD maintain excellent vision. Only in the most advanced cases of dry AMD do people experience significant visual loss. Even people with advanced dry AMD can typically see well enough to function quite well. Tasks that require good detailed vision like reading, driving and recognizing faces, however, are difficult. Unfortunately, there is no widely accepted treatment for dry AMD. Vitamins are typically recommended in an effort to stabilize the vision, however. See “Vitamins and Other Nutritional Supplements” below for a discussion of vitamins. The photograph to the left shows typical dry AMD. Notice the numerous yellow dots; these are deposits beneath the retina known as drusen and are a hallmark of dry AMD:
The following video further describes dry AMD:
“Wet” AMD is the growth of abnormal blood vessels beneath the retina. Although it causes visual loss much more often than dry AMD, only about 10% of AMD cases are wet. These abnormal blood vessels bleed and leak fluid under the retina; hence, the term wet AMD. You can think of the abnormal blood vessels like weeds. When these vessels bleed and leak fluid under the retina, the vision usually becomes blurred and distorted. Eventually, a scar often develops beneath the retina, causing severe visual loss. You can think of the scar like a large rock beneath the grass. Just as the grass would not grow, the retina does not function well with a scar beneath it. Like dry AMD, wet AMD only affects the central vision and does not affect the peripheral vision. A square containing many tiny boxes, called an Amsler grid, is often used to detect wet AMD in its earliest stages. The following video describes the Amsler grid and how it is used:
How is AMD treated?
Wet AMD typically causes more severe visual loss than dry AMD, when untreated. On the other hand, there are treatments available for wet AMD for limiting visual loss, whereas there are no treatments available for dry AMD, apart from vitamin supplements that may slow the progression of the disease. Below is a summary of treatments currently available for wet AMD.
1) Vabysmo (faricimab)
Vabysmo is the newest injectable medication for “wet” macular degeneration, approved by the FDA in 2022. Clinical trials that led to the approval of this medication suggested the drug may be more potent, resulting in less “leaking” of the “wet” macular blood vessels (it was also simultaneously approved for diabetic macular edema). This drug has a unique mechanism of action inhibiting two receptors simultaneously that are thought cause vascular leakage in the retina: VEGF and Ang-2. Patients may benefit from fewer required injections in the long-run with Vabysmo, with many needing treatments only once every 2-3 months, even beginning in the first year. Vabysmo is quite expensive, priced over $2,300 per injection.
2) Eylea (aflibercept)
Eylea is the next newest treatment option for wet AMD, which is also FDA approved. It is injected into the eye in the office, using the same technique that we use for the other injectable medications. Like Vabysmo, Lucentis, and Avastin, Eylea inhibits “VEGF”, a substance that causes growth of abnormal vessels behind the retina, but it accomplishes this task through a different mechanism. Eylea is quite expensive, priced over $2,000 per injection.
3) Lucentis (ranibizumab)
Lucentis was developed and FDA-approved specifically for wet AMD. When treatment is initiated, about three consecutive injections are typically administered, about one month apart. An attempt is often made to gradually lengthen the interval between injections, eventually spacing them a few months apart if possible. Lucentis has been found to improve the vision significantly in about 40% of cases and to stabilize the vision in about 90% of cases. Lucentis is quite expensive, priced over $2,000 per injection.
4) Avastin (bevacizumab)
Avastin was developed and FDA-approved for metastatic colon cancer, but it seems to be as effective as Lucentis at improving or stabilizing vision. A major study called the CATT (Comparison of Age-related Macular Degeneration Treatments Trials) was conducted to determine whether Lucentis and Avastin are, indeed, equally effective. The two-year results of the CATT show no significant difference in their effectiveness. In patients with colon cancer who receive high doses of Avastin by vein, there may be a slightly increased risk of complications such as stroke. Avastin does not seem to increase the risk of stroke when injected into the eye, however. About 1/500th of the typical colon cancer dose is injected into the eye, so very little of the medication reaches the bloodstream. Since the dose of Avastin is so tiny compared to the amount required for cancer treatment, Avastin is very inexpensive for treatment of wet AMD at about $30 per injection.
Vabysmo, Eylea, Lucentis and Avastin are known as “anti-VEGF” therapies. The following video describes anti-VEGF therapy for wet AMD:
4) Susvimo (Lucentis refillable intraocular implant)
Susvimo is a vascular endothelial growth factor (VEGF) inhibitor refillable intraocular implant indicated for the treatment of patients with wet Age-related Macular Degeneration (AMD). The implant is surgically inserted into the eye during a one-time, outpatient procedure. It is refilled with Lucentis during an in-office injection about every six months to maintain therapeutic levels of medicine. Supplemental injection treatments can be given if necessary. This treatment may be a good option for patients who require frequent injections.
5) Photodynamic therapy (PDT)
PDT was approved by the Food and Drug Administration in 2000. It was once the primary treatment for wet AMD but has been largely replaced by injectable medications. Some studies have indicated that combining PDT with injections can reduce the frequency of injections needed. However, there is some concern among retina specialists that visual outcomes may not be as good after combination therapy than with injections alone. PDT is intended for patients who have abnormal blood vessel growth beneath the very central part of the macula. The procedure involves the injection of a dye into a vein in the arm, followed by shining a low-intensity laser, sometimes called a “cold” laser, on the abnormal vessels for 83 seconds. This low-intensity laser “triggers” a photochemical reaction that damages the abnormal vessels, causing them to close. As a result, the bleeding and leaking stops. The following video further describes PDT:
6) Vitamins and Other Nutritional Supplements
AREDS (Age-Related Eye Disease Study) was a large study that found that specific doses of vitamin A, vitamin C,vitamin E and zinc can reduce the likelihood of progression to advanced AMD by about 25%. There has been some concern that the risk of lung cancer may increase if smokers take beta carotene, so a “smoker’s formula”, substituting lutein for beta carotene was developed for smokers (smoking, itself, is known to cause progression of AMD, so it is best to stop smoking).
AREDS2, the follow-up study to AREDS, has made some major findings: 1) Lutein and a lesser-known supplement called zeaxanthin help to reduce the probability of visual loss from macular degeneration; 2) omega-3 fatty acids (often found in fish oil) do not appear to reduce the likelihood of visual loss from macular degeneration; and 3) beta carotene increases the risk of lung cancer in former smokers as well as current smokers. Based on AREDS2, it appears that the substitution of lutein and zeaxanthin, along with the omission of beta carotene and omega-3 fatty acids, are advisable. The formula currently recommended, then, contains lutein, zeaxanthin, vitamin C, vitamin E, and zinc.
7) Low Vision Aids
Even though AMD can cause severe visual loss, special devices can be used to make the most of the vision that remains. A variety of low vision aids are available to assist with activities like reading. These include various types of magnifying glasses and closed-circuit televisions. Resources for low vision assistance can be found in our Helpful Links. Below is an example of a closed-circuit television that can help patients with severe visual loss from macular degeneration to read:
Telescopic lens implants are FDA-approved and can improve the vision in patients with advanced AMD. These implants are placed in the eye in a manner similar to intraocular lens implantation during cataract surgery.



